Top News
Optum shuts down its virtual-first urgent and primary care service, three years after it formed Optum Virtual Care during the pandemic’s peak days.
The company had added a discounted prescription-writing and refill service as part of Optum Perks in January 2024.
Reader Comments

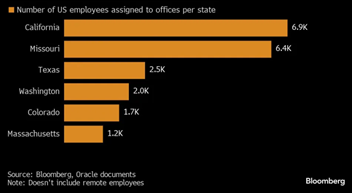
From Oracle of Delphi: “Re: Oracle. Larry Ellison seemed to be riffing off-script when he announced that the company would relocate its headquarters to Nashville.” The company has been holding various events in the city and Larry now says it’s important for the company to be located in healthcare-centric Nashville. He made that surprising announcement during a fireside chat at the company’s healthcare conference, which must have driven its unprepared PR people crazy. I’m surprised that the tiny Cerner tail is wagging the massive Oracle dog, especially since the company – other than Larry – mostly complains that the former Cerner business is not profitable enough, while also surely thinking but not saying that Epic is eating its lunch. The headquarters role is somewhat symbolic, given that Oracle has just 4,000 of its 164,000 employees housed in Austin following its 2020 HQ relocation to there from Silicon Valley. My takeaways:
- This is Larry talking, not an official company announcement. What Larry says doesn’t always happen.
- It could be that the company just wants to take a dig at Austin for some reason or is just incentive-milking given the prestige of having Oracle’s HQ in their city.
- While Ellison said in his surprise proclamation that “Nashville is a fabulous place to live” (note: he doesn’t live there), employees may not be happy to be forced to move there, especially since many of them just moved from California to Texas.
- It’s probably not unrelated that both Texas and Tennessee don’t have state income tax and that quite a few companies are bailing on Austin because of cost that has been driven by high growth.
- I’ll be curious how and when Oracle’s PR people spin this and how quickly the company actually seals the deal by buying or building a headquarters campus.
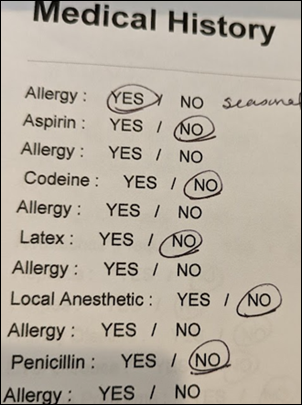
From Panama Hat: “Re: obtaining your own health records. I am an advanced practice nurse and have had significant issues obtaining my own health records. Especially with M&A, outsourcing HIM request to outside companies, and the lack of access to actual humans. I wonder if in-house IT teams created work flows of the antiquated process involved and validated them afterwards, especially after the hospital merged or outsourced some HIM services.” I don’t have recent experience, although I detailed my frustration with the patient-hostile process way back in 2016, which included a compliant to OCR that they closed in saying that they had provided “technical assistance to the hospital.” Perhaps new information blocking provisions will scare foot-dragging hospitals into doing the right thing and eliminating idiotic policies that require patients to explore the hospital basement to find HIM so they can fill out a paper form in person, or Google an online fax service to (ironically) request electronic copies of their own information. Readers, I would be delighted to hear about your recent experience in obtaining copies of your records, especially if you are still mad about it.
From Mailman: “Re: Epic shutting down data exchange with Particle Health customers that are using it for non-treatment purposes. The wildest example was Integritort, where class action lawyers were using Particle to pull down real-time medical records for lawsuits.” Particle founder Troy Bannister posted a self-righteous LinkedIn diatribe against Epic for closing access to some questionable Particle customers who seemed to be using patient data for non-treatment purposes (which isn’t allowed), but I haven’t heard a peep from him since. My takeaways: (a) it’s pretty easy for Epic to compare which entities are downloading data without sending any back to Epic, which would suggest that those users aren’t actually treating patients; and (b) struggling startups will push ethics aside in favor of plausible deniability (“we didn’t know that our clients were doing anything wrong”) if they gain revenue or investment. Bannister said when he left the company as CEO a year ago that its goal was being refocused to “creating as much value as possible from the growing amount of data we have access to,” which says a lot about trusting startups with healthcare data.
From List Sucker: “Re: Newsweek’s list of best digital health companies. Review their methodology.” Most healthcare company lists are pure clickbait, paid company promotion, or some “content writer” trawling the Internet to make up a worthless and often laughable list (anyone who refers to their pitiful intellectual output as “content” is just trying to fill space for cash). Newsweek’s list of “best” companies looked at financial performance (which is obviously not much of a metric for privately held companies that self-report), website and app traffic data (which is clearly irrelevant), and whatever input Holon IQ chose to provide (its own lists seem to use self-nomination in the absence of auditable company-provided numbers). All companies love being named to “best” lists, even when the award comes from someone who is too ashamed of their criteria to list them, and handing over cash to make the list is not uncommon. The good news is that absolutely nobody cares except company marketing people who report their big win like it came from careful analysis.
From Disruptive Behavior: “Re: readers’ list of realistic first steps to improve US healthcare. Unfortunately ‘realistic’ change means that Congress doesn’t have to act, industry incumbents won’t have their revenue or power reduced, jobs aren’t reduced, and nothing runs afoul of capitalism or the Constitution.” I agree, which is why throwing out great but entirely unlikely options like universal health insurance doesn’t get us anywhere. In the US, healthcare is a right for everyone who sells it.
A recap of Oracle Health Summit this week in Nashville from an attendee
- Seema Verma said that Millennium will be at the center of Oracle Health’s offerings. Product roadmaps have been published, although they didn’t provide them to this group.
- Upcoming products: a payment solution, Oracle Clinical Digital Assistant (expected to GA in a couple of months), public APIs of unspecified variety (addition FHIR APIs, polished up versions of Cerner’s existing ones, use cases not specified).
- HealthIntent has been rebranded as Oracle Health Data Intelligence and has new functionality and user interface.
- A new patient portal will be released this year, with the company saying they have pulled ideas from food and beverage and retail industries.
- Larry Ellison let it slip – accidentally or otherwise – that Oracle’s headquarters will “ultimately” be moved to Nashville. He said it will have a community clinic, a concert venue, a lake, and a pedestrian bridge over the river that will connect the campus to downtown Nashville.
- Ellison took shots at AWS, saying that the Change Healthcare breach wouldn’t have happened if they had been on Oracle Cloud and autonomous databases.
- He says that 50% of Cerner customers have moved to Autonomous Cloud in Oracle Cloud infrastructure.
- The company will add gene sequencing technology to PathNet.
- Ellison says that passwords will be eliminated in all Oracle systems by the end of the year, replaced with passcodes and other authentication methods.
- EVP Mike Sicilia says that the company will focus on a constant stream of incremental improvements rather than large releases and upgrades.
- The consistent theme of attendees per this individual is that Oracle has made big promises and delivered little. Compared to Epic UGM, this meeting had few customers placed front and center, it didn’t offer tangible product previews, and attendees found little to take back home as action items. Oracle had some big names on the panels who tried to seem visionary. Big execs like David Feinberg and Mike Sicilia were accessible and mingling, but that might have been because it was only around 500 attendees.
Thoughts on the FTC’s ban on companies forcing employees to sign non-compete agreements
I received more reader feedback on this topic than any in recent memory. I’ll summarize their thoughts and mine:
- FTC says that 45% of US physicians – as opposed to 20% of American employees in general — are working under non-compete agreements and estimates that healthcare costs will be reduced by $194 billion over 10 years by eliminating them.
- The FTC’s decision will certainly be challenged. It wouldn’t surprise me if Epic gets involved.
- The American Hospital Association loathes the idea, declaring it “bad law, bad policy, and clear sign of an agency run amok” that has ample legal precedent to be challenged. They are particularly galled that FTC would dare regulate “certain tax-exempt, non-profit organizations” whose multi-million dollar executives are among the worst offenders of interfering with a free job market for clinicians to expand their regional and national empires by smothering competitors.
Highlights of the rule:
- It takes effect 120 days after being published in the Federal Register, at which time all existing non-competes – except for those of senior executives who make more than $150,000 and are involved in corporate policy-making – are no longer enforceable. Physicians cannot be excluded from the regulation just because they are highly paid, although health systems might argue that they are involved in corporate policy-making through their medical staff policy involvement.
- FTC urges companies to notify current and former employees that their non-compete clauses are no longer valid.
- FTC clarifies that the popular myth that FTC has no jurisdiction over non-profits is incorrect. It notes that a healthcare system can’t simply hide behind its non-profit IRS status, saying that it will go after organizations that were set up specifically to offer benefits to stakeholders or that have partnered with a for-profit company that gains control of the business. It also says IRS has rejected the non-profit claims of non-profits that pay excessively to executives, founders, board members, families, and other insiders.
- FTC cites precedents by some states that have banned non-competes. It estimates that 58% of non-profits and 19% of government-operated hospitals will likely be covered by the final rule. Its research found that non-competes are almost always used specifically as an unfair method of competition.
- Workers who are contracted by non-profit hospitals from a for-profit staffing company or physician group are explicitly covered by the policy. Their employer can’t use non-competes and their assigned work location is irrelevant.
- FTC says that non-profit health systems that manage to escape FTC jurisdiction will still suffer “self-inflicted damage” because while they can continue to trap current employees with non-compete threats, they will have a tough time recruiting.
- The rule takes a direct shot non-profit health systems that “are operating to maximize profits, paying multi-million-dollar salaries to executives, deploying aggressive collection tactics with low-income patients, and spending less on community benefits than they receive in tax exemptions.”
Additional comments about Epic:
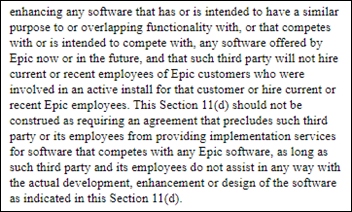
- The company, which requires employees to sign some of the industry’s most restrictive non-compete agreements, has no way to wiggle around this policy as it is currently written.
- However, FTC ruling aside, Epic still controls where former employees (both their own and those who work for client hospitals) can take software-related jobs by controlling access to UserWeb, ongoing training, and certification. It would be difficult for an Epic employee to mount a long-expensive legal challenge of these internal company decisions. If Epic doesn’t want you working for an employer that is included on its long length of “competitors,” you will have a tough time getting hired there regardless of FTC’s proclamations, at which time your only legal recourse is to hire your own attorney to face off against Epic’s. Potential hirers don’t want to poke the Epic bear and FTC rulings won’t change that, except possibly in the part of the rule that prohibits any activity that would prevent worker from seeking a new job or starting a new business (which makes it even more likely that Epic will get involved in the legal debate).
- I believe that Epic’s client contracts preclude their hospitals from hiring employees from other Epic sites except under specific conditions or approvals. I don’t know if those terms violate the FTC’s regulation since the agreement is between the two companies, with no involvement and perhaps no knowledge by the employee.
Healthcare impact, assuming that the regulation stands after inevitable challenges:
- A huge chunk of America’s doctors and other clinician can now change jobs freely and will likely do so. Health systems can no longer strong-arm them into staying and instead had better start addressing their clinical and employment issues since a hospital without doctors and nurses is just a massively expensive, poorly run hotel.
- Doctors who are disgruntled at being stuck working for Optum or other companies that bought their employers are free to leave the building.
- The worst outcome would be if lobbyist-heavy “non-profit” health systems manage to evade the rule and for-profit medical practices don’t, which would allow hospitals to continue to kill off private practices. FTC’s estimate that up to 40% of hospitals don’t fall within their jurisdiction is troubling.
- The regulation calls into question the practice of health systems with multi-billions of dollars in revenue, executive offices filled with million-dollar employees, and market control that spans ever-widening geographic areas should be allowed to hide as non-profits under IRS rules and therefore tie their current stable of doctors to existing agreements to prevent them from taking better jobs.
- Vendors and start-ups will be challenged to see their IP walking out the door in the form of free-market employees who move to competitors mostly because of what they know about their former employer. They are also free to start their own competing firm in using that information.
- Companies can continue to use non-disclosure and confidentiality agreements to protect their IP, and the wording and deployment scope of those might be expanded.
- It’s a good time to be a healthcare recruiter, especially of physicians.
Lawyers or policy wonks – what will FTC’s enforcement mechanism be? Does it have to sue the violator, or will the employee have to file their own lawsuit and then have FTC join? Assuming it can address civil contempt and civil penalty actions, how likely is FTC to quickly intervene with and then resolve the large number of employee complaints that it will receive? Hospitals don’t worry too much about most regulatory issues that don’t involve CMS payment threats, especially if the financial benefit of ignoring the requirement is greater than paying the fine.
HIStalk Announcements and Requests
Three companies reached out in the past week to ask about their sponsorship, only to find that it expired long ago because our company contact had left and nobody else returned our reminder emails. Hint: if your company isn’t listed under Sponsor Quick Links on the right side of the desktop version of the web page, you aren’t a sponsor. Fortunately, the fix is simple — contact Lorre.
I focus on reporting industry news instead of creating videos, podcasts, or self-congratulatory social media campaigns. However, I might be overlooking the value of using LinkedIn to stay in touch with HIStalk readers. Question: if you were me, would you hire someone part-time or contract who knows LinkedIn well to more actively use that channel, even if they aren’t health IT experts? I don’t like the idea of just shouting “Hey, I’m here” in hopes of drawing clicks, but perhaps some of what I’m already doing could be made more accessible there.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
98point6, which previously operated as a virtual primary care provider and then sold that business to Transcarent to focus on selling its software, lays off what appears to be most of its employees who remained after previous headcount reductions. The company bought chat-based telehealth provider Bright.md in January 2024 and had raised $300 million of venture capital investment as of early 2023.
Walgreens launches a $24 billion annual revenue specialty pharmacy that will add gene and cell services to its AllianceRx specialty and home delivery business.

Epic breaks ground on its sixth campus called Other Worlds, which draws inspiration from “The Lord of the Rings” and “The Chronicles of Narnia.” The company has 13,000 employees, up 40% over the past six years. New buildings will open this year in its Storybook and Wizards Academy campuses. Interesting: 80% of employees work in individual offices, with the remainder sharing two-person offices, and each office has its own thermostats and windows that open. Also interesting: the company calls its whimsical decorating style “cheap and cheerful,” as it doesn’t cost more to choose colorful paint and carpet and its “cozy spaces” are decorated with thrift store furniture.
Sales
- National reference laboratory ARUP Laboratories will implement Ellkay’s LKOrbit to support its clients in ordering, results delivery, and collecting billing information.
People

Clover Health hires Peter Kuipers, MBA (Omnicell) as CFO.

Linda Stotsky (Boston Software Systems) joins ClinicMind as chief marketing officer.

Prominence Advisors hires Mark Ostendorf, MBA (DrFirst) as chief revenue officer.
Announcements and Implementations
Innovar Healthcare announces an OSS Mirth Connect plug-in that adds OpenAI technology for task automation.
Truveta publishes a mother-child EHR dataset for research, which includes clinician notes and images from 30 health systems that are linked to claims, SDOH, and mortality data.

A new KLAS report looks at CRM, finding that Best in Class winner Innovaccer’s clients are highly satisfied even though it’s the newest CRM market entrant and its user base is small. Epic is seeing increased adoption of Cheers, although nickel-and-diming issues have been reported. Salesforce has the largest market share, but respondents question its value and 60% of them gripe about extra fees for training, support, implementation, and new functionality.
Government and Politics
Seattle Children’s Hospital, which sued Texas Attorney General Ken Paxton for demanding what it says is a “sham” investigation into transition gender care provided to Texas residents, says that the AG’s office has withdrawn its demands for patient-level information. Paxton declared the dismissal as a win, saying that his questions led the hospital to forfeit its registration to do business in Texas.
ONC publishes Common Agreement Version 2.0, which provides updates for FHIR APIs.
California has spent $500 million to offer young people free, app-based virtual counseling sessions for behavioral health issues, provided by BrightLife Kids and Soluna. Response has been close to non-existent – only 0.1% of those who are eligible have even signed up and one company has missed its committed date to deliver an Android version. The state has declined to say how many of those 15,000 registrants have actually engaged with the apps and no schools are promoting their use. Some experts are concerned that the companies – one VC backed, the other publicly traded – sometimes use unlicensed coaches who might miss problems that should be referred to clinicians.
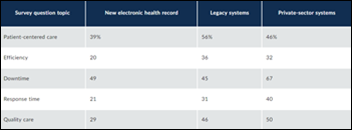
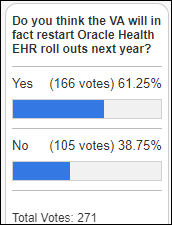
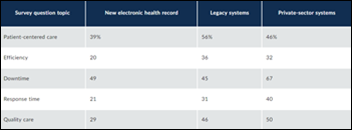
A GAO report says that DoD and VA will not likely reach the integration goal that was set at the jointly operated and newly live Lovell Federal Health Care Center. GAO also finds that DoD user satisfaction is lower with the Oracle Health system than for the legacy systems it replaced as well as private sector systems. GAO also found that years-old problems remain with the Henry Schein Dentrix dental module, to the point that DoD is looking to replace it.
Other
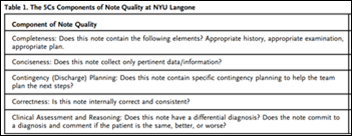
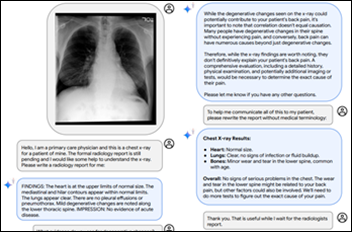
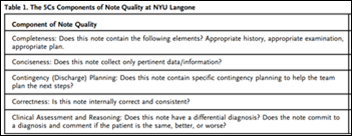
A NEJM Catalyst case study from NYU Langone Health finds that AI can help improve poor clinical note quality, also noting that the real challenge is that (a) no universal standard exists for measuring note quality, leaving it up to each organization to define their own standards; and (b) peer-to-peer review of notes organizationally doesn’t scale well. The organization developed components of note quality, then trained AI to grade them by the thousands to perform quality reporting, identify physicians who could benefit from peer feedback, evaluate the impact of new templates and educational interventions, and assess individual performance. The organization also provides data review links to minimize note bloat that was caused by text tables. This is good work because instead of just using AI to summarize a chart or facilitate voice-to-text enhancement to create the same note that could have been done manually, it takes a bigger swing in laying out AI-measurable note quality standards.
It’s Y2K all over again: a 101-year old woman must fly commercial as an “unescorted minor” because airline booking systems translate a birth year of 1923 to 2023.
The times in which we live: Vancouver Island Health Authority tells hospital nurses to allow patients to use illicit drugs in their rooms and suggests that they teach patients to inject their personal stash into their IV lines, extending previous requirements for nurses to offer them crack pipes and matches.
Sponsor Updates

- Healthcare IT Leaders staff conduct a used clothing drive for the No Longer Bound Thrift Store in Atlanta.
- KLAS Research highlights Agfa HealthCare in its new “Enterprise Imaging Report 2024: Vendors and Providers Driving Market Progress.”
- First Databank’s Targeted Medication Warnings earns Epic’s Toolbox designation in the Medication Dosing Decision Support Toolbox category.
- DrFirst will combine its prescription fill data with remote monitoring data from PatchRx to equip providers with the data they need to improve patient medication adherence.
- MRO extends its automated retrieval services by automating data exchange between providers for continuity of care purposes.
- Marshfield Clinic Health System honors Findhelp with its 2023 Outstanding Partner in Community Health Award.
- FinThrive publishes “The Complete Guide to Prior Authorizations.”
- HealthMark Group will present at the American Alliance of Orthopaedic Executives Annual Conference April 26 in Chicago.
- Konza National Network welcomes Wichita Surgical Specialists to the Konza QHIN.
- Medhost publishes a new white paper, “A Guide to Finding a Secure EHR Hosting Service.”
- Meditech works with the Massachusetts Association of the Blind and Visually Impaired to test the accessibility of the Expanse Patient and Consumer Health Portal for the blind and visually impaired.
- Net Health will host its inaugural Net Health Next Customer Conference May 9 in Tampa Bay, FL.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.


































1) RE: EMR down & good staff collaboration. I believe it. Having worked at a now defunct EMR for 15+…